 |
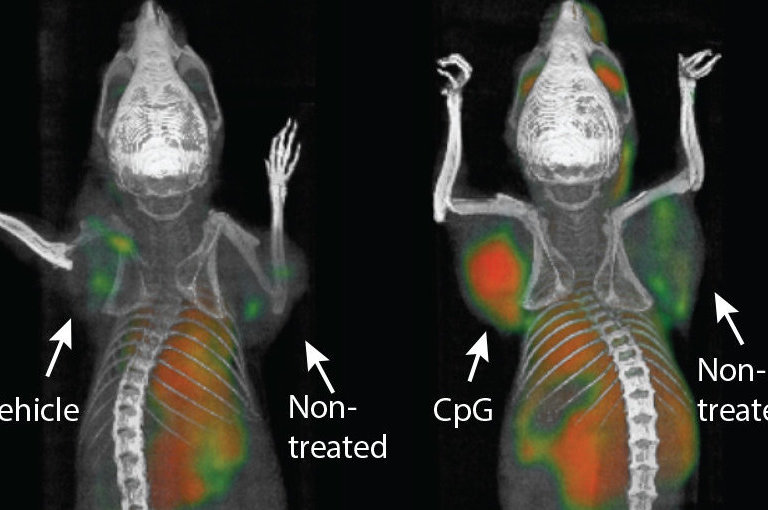
| Scientists devised a pinpointed immunotherapy regimen that eradicated tumors throughout the body in mice. |
For decades, scientists have been chasing a cancer “vaccine” that wakes the sleeping army of immune cells and trains it to attack cancer. Now a new technique has scientists injecting microdoses of immune-boosting agents directly into cancerous tumors, which appears to not only kill the targeted tumor, but eradicate similar tumors elsewhere in the body — at least in mice.
In a preclinical study published in Science Translational Medicine, 90 mice with multiple transplanted tumors were injected with two immunotherapy agents, and in 87 cases, all signs of cancer were wiped out.
The promising results, reported by Ronald Levy at the Stanford University School of Medicine, provide further hope that immunotherapy is the future of cancer treatment. Instead of bombarding the body with high doses of toxic chemicals and radiation, we can recruit our own immune systems to fight back.
In Levy’s two-step cancer vaccine, a short stretch of DNA called a CpG oligonucleotide was first injected into the tumor site. CpG is something called a Toll-like receptor, a special kind of immune system protein that recognizes invading pathogens.
When micrograms of this protein (millionths of a gram) were injected into the mouse tumors, they activated the expression of a receptor called OX40 on nearby T cells that had originally swarmed to the tumor site, but had been rendered inactive.
The second injection contained an antibody that attached to those newly activated OX40 receptors and essentially turned the T cells back “on.” Before their activity was suppressed, those same T cells were primed to respond to the precise antigens produced by the tumor. With a boost from the vaccine, now they were back in action.
The mice in the Stanford experiment were transplanted with lymphoma tumors, but Levy said in a statement that the vaccine achieved similar results with breast, colon, and melanoma tumors. Even more impressive was that some of the reactivated T cells circulated throughout the body and attacked tumors far from the injection site.
“When we use these two agents together, we see the elimination of tumors all over the body,” said Levy. “This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Levy was referring to other emerging immunotherapy cancer treatments like CAR-T therapy, in which a patient’s T cells are removed and genetically altered to carry custom-made antigen receptors for the patient’s particular type of cancer. And checkpoint inhibitors, a therapy that targets specific immune system proteins that allow cancer cells to hide in plain sight.
Another promising immunotherapy uses the listeria bacteria as a vector to deliver tumor-specific antigens to the entire immune system.
The listeria technique was developed by Yvonne Paterson at the University of Pennsylvania School of Medicine and has been licensed by Advaxis Immunotherapies, which is already testing its vaccine formula in phase 3 human trials for certain types of late-stage cancers. The Stanford team just began recruiting its first 15 human patients.
Reached by email, Paterson called Levy’s paper “a very nice preclinical study that shows the power of expanding and activating pre-existing tumor-specific T cells that accumulate in tumors but are not able to control tumor growth.”
One disadvantage of the direct-injection technique, said Paterson, is that it’s limited to tumors that are easily accessible.
“One can see how his approach might work in the human equivalents of lymphoma, breast cancer and also in melanoma, where there is surface accessible tumor,” add Paterson. “However, there are many cancers to which it might not be very applicable.”
Levy is a pioneer in the immunotherapy field, winning FDA approval in 1997 for the first lab-designed antibody to be used in conjunction with traditional chemotherapy. But Levy is not the first to experiment with immune-boosting vaccines that target T cells closest to the tumor site.
Read more at Seeker
No comments:
Post a Comment